Consistent Mask Use and SARS‐CoV‐2 Epidemiology: a simulation modelling study
Masks effectively reduce severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) transmission.1 However, the impact of mask wearing over an extended period on morbidity and mortality at the population level is less clear, particularly given the interplay between mask effectiveness, population immunity, and other public health and social measures.
We recently reported the results of an integrated epidemiologic and economic agent‐based model that assessed the costs and benefits of more than one hundred coronavirus disease 2019 (COVID‐19) control policies used in Victoria, in combination with nine scenarios of SARS‐CoV‐2 variant emergence, during the eighteen months from April 2022.2 We included mask interventions implemented only during large epidemic waves that increased both general mask wearing and the proportion of mask wearing that involved respirators (eg, N95 masks). These policies had minimal impact on health outcomes.2 For this study, we extended these analyses to determine the impact of age‐stratified consistent community‐level mask wearing (ie, at all times when outside the home) on numbers of SARS‐CoV‐2 infections and COVID‐19‐related deaths.
We modelled different levels of consistent mask‐wearing by people under 60 years of age (none, 20%, 35%, 50%; lower proportions were applied to people under 20 years of age: see footnote to Box 1) together with equal or greater levels of mask wearing by people aged 60 years or more (about 20% of the population),3 to a maximum of 75%. At each level of use, 80% of masks used were assumed to be cloth or surgical masks and 20% to be respirators. Other public health and social measures were fixed. The model began in April 2022 with Omicron BA.1 and BA.2 as the dominant SARS‐CoV‐2 variants, with the gradual emergence of BA.4 and BA.5 from May 2022. We calculated quarterly and cumulative median numbers of infections and deaths (from 500 model runs for each scenario, allowing for stochastic and input parameter uncertainty) during the twelve months from April 2022. Odds ratios for the relative risk of infection for people exposed to an infected person (wearing a mask v not wearing a mask) were set at 0.47 for cloth and surgical masks and 0.20 for respirators1 (further model details: Supporting Information, supplementary methods). As we used publicly available data, we did not seek formal ethics approval for our study.
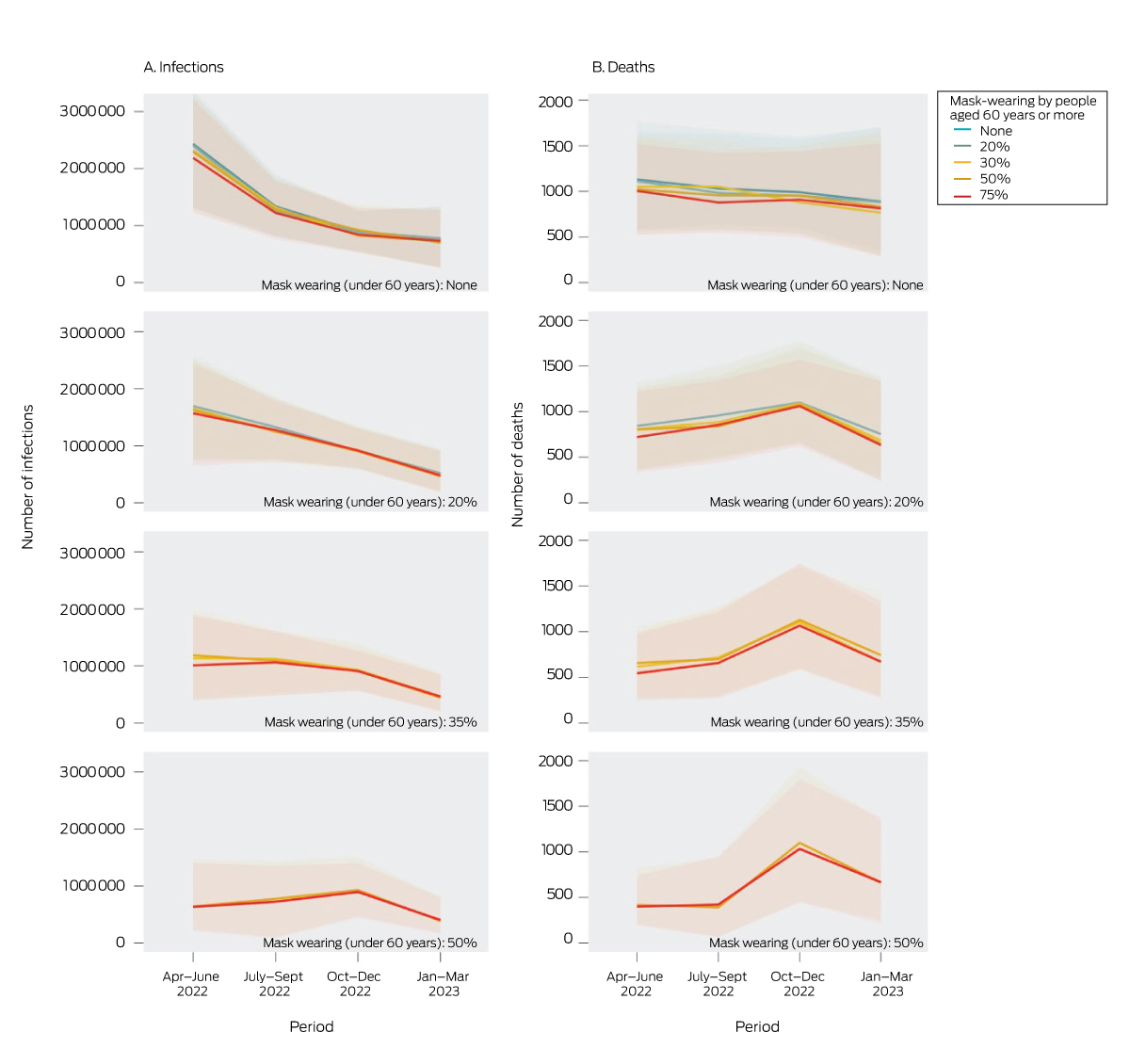
Compared with no mask wearing, consistent mask use by 20% in both age groups (under 60 years, 60 years or more) reduced the median number of infections by 16.4% (uncertainty interval [UI; 5th to 95th percentiles], –30.4% to +2.7%) and the median number of deaths by 10.6% (UI, –33.0% to +20.7%). Increasing mask wearing in both age groups to 50% reduced infections by 38.4% (UI, –96.0% to –6.7%) and deaths by 25.8% (UI, –97.0% to +26.1%). The effects at any given level of mask wearing by people under 60 were not markedly influenced by the level for people aged 60 years or more (Box 1). The largest reductions in infection and death numbers achieved were during the first quarter of the modelled time period (Box 2). The rise in the numbers of deaths during the third quarter may be related to reduced infection‐derived immunity following lower viral transmission earlier in the model run; however, the cumulative infection and death numbers were still lower for these scenarios than with zero mask wearing. The effects of mask wearing on COVID‐19‐related hospitalisations were similar to those for infections and deaths (Supporting Information, table 5).
Box 2 – Modelled quarterly numbers of infections and deaths in Victoria, April 2022 –March 2023 (based on 500 model runs with separate draws of input parameters), by mask wearing levels for people under 60 years and those aged 60 years or more*
As our model specified that older people have fewer contacts with others, but not the probability of contact with people from specific age strata, we may have underestimated the impact of protecting older people by specifically increasing mask use by people aged 60 years or more. Further, the uncertainty intervals for our modelled outputs are quite broad. This is the result of input parameter uncertainty, including for estimated mask effectiveness (Supporting Information, supplementary methods), and stochastic uncertainty (our model included only 5000 agents). Finally, our mask effectiveness estimates were based on the findings of a single study.1 The literature on mask effectiveness is highly heterogeneous,4 and the topic requires further, high quality research.
The net impact of mask wearing will vary according to the levels of other interventions, including vaccination rates. Nevertheless, our findings suggest that consistently higher mask wearing rates across all ages would reduce the cumulative infection and mortality burden in Victoria.